The emphasis in ischaemic heart disease (IHD) diagnosis has historically been directed towards the identification of epicardial coronary stenosis by selective coronary angiography, and its management by percutaneous coronary intervention (PCI) or coronary bypass graft surgery. Over the past two decades, the application of coronary physiology techniques to identify the haemodynamic severity of epicardial coronary stenoses to guide decision-making regarding revascularisation has evolved into an indispensable part of IHD management.1 This is mainly attributable to the finding that routine PCI of stenoses deemed significant by coronary angiography (>50 % diameter stenosis) does not lead to improved patient outcomes beyond swift alleviation of angina pectoris.2 The introduction of fractional flow reserve (FFR), a coronary pressure-derived estimate of the impact of the coronary stenosis on coronary flow, has played a pivotal role in this regard.3–5 FFR-guided coronary intervention has been documented to provide equivalent functional and long-term clinical outcomes of IHD management compared with an angiography-guided approach, while reducing the number of revascularisation procedures.6 The results of the pivotal Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME I) and FFR-guided Percutaneous Coronary Intervention plus Medical Treatment versus Medical Treatment Alone in Patients with Stable Coronary Artery Disease (FAME II) studies have led FFR to be endorsed by revascularisation guidelines with a class I level of evidence A recommendation in the setting of stable IHD with angiographically equivocal disease severity and absence of noninvasive documentation of myocardial ischaemia.1 However, the results of the FAME II study, evaluating the benefit of PCI over guideline-directed medical therapy in vessels with an abnormal FFR-value, indicate that over 80 % of patients with abnormal FFR do not suffer from adverse events, while 60 % of these patients did not require PCI during a two years follow-up period.7,8 The finding that a dominant proportion of FFR-positive vessels may not require revascularisation to improve clinical or functional outcomes is confusing in an era when strict adherence to obtained FFR-values is advocated in clinical practice guidelines. The origin of these findings is, at least, partially explained by the difference between coronary pressure-derived estimation of coronary flow impairment due to a stenosis and direct measurement of coronary flow for this purpose.9 This review details the fundamental basis of clinical coronary physiology, and how this relates to the evaluation of coronary stenosis using coronary pressure or coronary flow.
Coronary Pressure-flow Relations: Autoregulation and Metabolic Adaptation
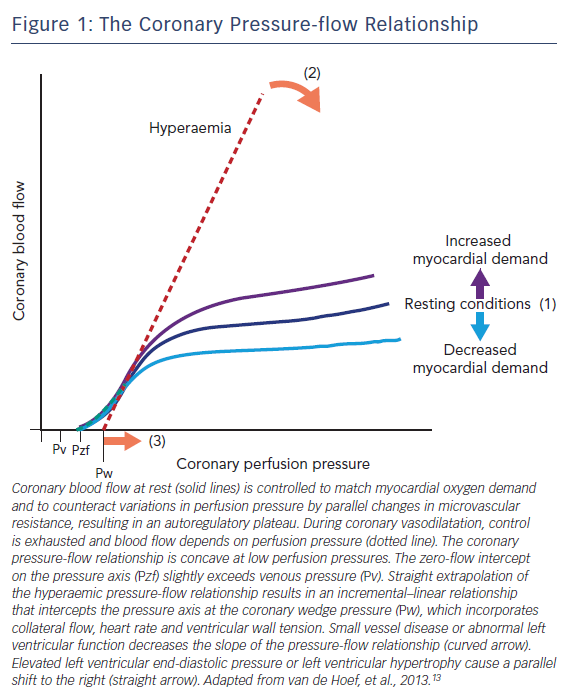
Figure 1 illustrates the fundamental coronary pressure-flow relationship. At a given level of myocardial demand, coronary flow remains relatively stable within a physiological range of perfusion pressures. This phenomenon is illustrated by the flow plateau in Figure 1, and is termed coronary autoregulation.10,11 An increase or decrease in myocardial demand leads to a parallel shift of the pressure-flow relationship, which is a process termed metabolic adaptation.10,11 Autoregulation and metabolic adaptation together maintain stable coronary flow at a level that meets myocardial demand. Put simply, these processes occur through compensatory adaptation of the coronary resistance vessels, which may vasodilate or vasoconstrict to adapt to perfusion pressure changes or changes in myocardial demand.12 The ability of the coronary resistance vessels to accommodate to such changes can be abolished by the use of potent coronary vasodilators, such as adenosine, papaverine or regadenoson, which override autoregulation by inducing pharmacological vasodilation of the coronary resistance vessels.10,11 Therefore, at maximal vasodilation, the coronary circulation cannot adapt to pressure or metabolic changes, and is perfusion pressure-dependent: an incremental-linear relationship between coronary pressure and flow occurs.13 Note that the relationship is linear, as the relationship is represented by a straight line, but this relationship is not proportional: the relationship does not pass through the zero-pressure intercept. The course of this pressure-flow relationship at maximal vasodilation is variable both within and between patients.14 The zero-pressure intercept is, among others, influenced by changes in heart rate, left ventricular filling pressures and myocardial hypertrophy.10 Similarly, the slope of the pressure-flow relationship in the individual patient changes, among other conditions, in the presence of small vessel disease or abnormal left ventricular function.15,16
Stenosis Physiology as the Basis for Stenosis Assessment
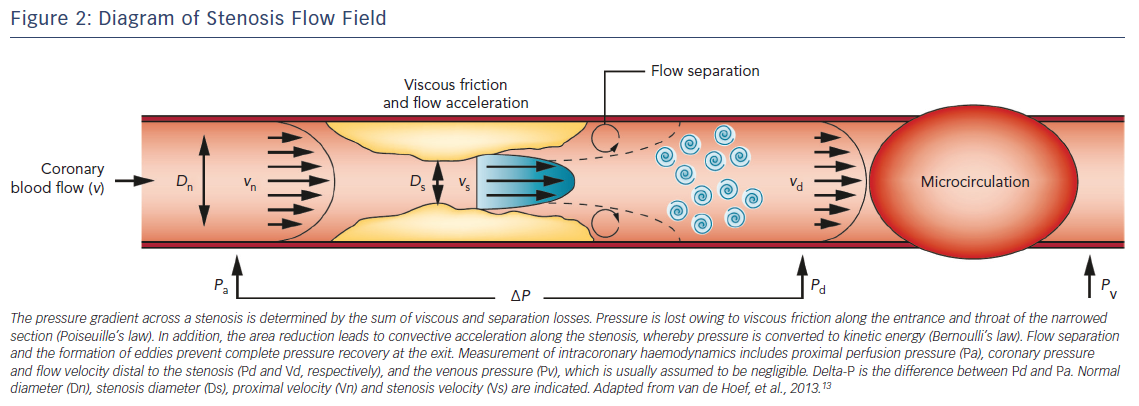
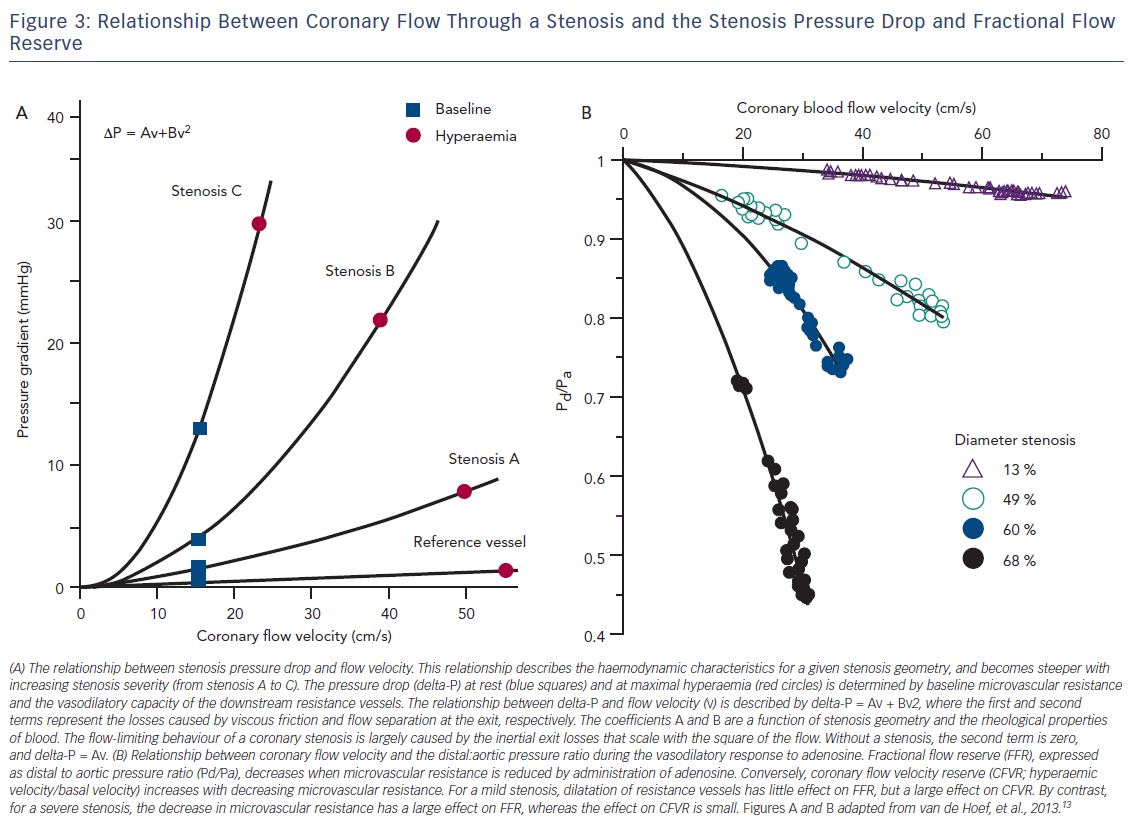
Figure 2 and Figure 3A illustrate the basic physiological behaviour of epicardial coronary stenosis. The pressure loss across a coronary stenosis not only depends on the severity of coronary narrowing, but to a large extent on the magnitude of flow that goes through the coronary artery.17,18 This pressure loss is due to viscous friction losses across the throat of the lesion, and separation losses that occur through acceleration of flow through the stenosis and the formation of eddies at the stenosis exit. Due to the combination of these effects, the pressure loss incurred by a stenosis increases quadratically with an increase in coronary flow (Figure 2A). For the application of coronary physiology in clinical practice, it is important to realise this implies that distal coronary pressure (thus, FFR) decreases (does become more abnormal) when coronary flow through the coronary artery increases (Figure 3B). As such, a severe decrease in coronary pressure can occur with low FFR-values merely due to the presence of high coronary flow. The clinical relevance of decreased coronary pressure in the presence of maintained coronary flow is debated, with studies documenting a relative high prevalence of this phenomenon and suggesting a benign character with favourable clinical outcomes.19,20 This agrees with early experimental findings documenting that decreased coronary pressure of the coronary circulation does not lead to evidence of myocardial ischaemia as long as coronary flow remains stable.21 The opposite of this phenomenon also occurs frequently, where a stenosis is associated with only limited decreased coronary pressure, merely due to the fact that coronary flow does not increase upon pharmacological vasodilation.19,20,22 This may occur in the setting of microvascular disease, or in the setting of focal stenosis superimposed on diffuse epicardial and/or microvascular disease. This phenomenon has been linked to impaired clinical outcomes, which suggests that the sole use of coronary pressure in practice may underestimate the clinical relevance of these stenoses.20,22
Coronary Flow for Stenosis Evaluation
Since the myocardium thrives on coronary flow to exert its contractile function,9,21 and coronary flow is the critical determinant of myocardial ischaemia,23,24 it seems self-evident that the evaluation coronary flow provides an important tool to identify haemodynamically relevant stenoses. The most widely studied flow-based index for this purpose is the maximal increase in coronary flow that is available upon an increase in myocardial demand: the coronary flow reserve (CFR).17,25 CFR is defined as the ratio of flow during maximal vasodilation to flow during resting conditions, and thereby reflects the reserve vasodilator capacity of the coronary resistance vessels. CFR can be assessed by either the Doppler flow velocity or coronary thermodilution technique.26,27 Doppler flow velocity can be assessed using a Doppler sensor-equipped guide wire and provides the operator with both average flow velocity values as well as the coronary flow velocity profile. Such assessment of Doppler flow velocity has the advantage that its magnitude is intrinsically corrected for the amount of perfused myocardial mass in the arterial distribution by the laws of normalised shear stress, and is therefore relatively independent of perfused myocardial mass.28,29 Coronary thermodilution can be assessed with a temperature-sensitive guide wire using rapid injections of room-temperature saline to obtain mean transit times of the saline boluses. These transit times are inversely relative to absolute coronary flow and allow to calculate CFR. Although CFR is not impacted by myocardial mass-dependence of coronary thermodilution, it is important to realise that absolute mean transit time values are influenced by the amount of subtended myocardial mass.30 Moreover, coronary thermodilution measurements require forced quick injection of room-temperature saline, which may affect coronary haemodynamics and may therefore affect flow values particularly during non-vasodilated conditions.31 Finally, coronary thermodilution requires a hyperaemic plateau phase to provide sufficient time for the repeated saline boluses, which is usually obtained using intravenous adenosine infusion. However, intravenous adenosine infusion frequently leads to a decrease in blood pressure. Since maximal coronary flow at coronary vasodilation depends on coronary perfusion pressure, such decreases in blood pressure due to intravenous adenosine infusion lead to lower maximal flow values and underestimation of CFR if not accounted for. Doppler velocity measurements can, in contrast, also be performed using intracoronary adenosine administration, which circumvents this issue. Nonetheless, despite its potential advantages, Doppler flow velocity measurements are considered more technically challenging than coronary thermodilution measurements.
With increasing stenosis severity, the coronary circulation compensates by progressive vasodilation of the coronary resistance vessels to maintain coronary flow at a level that meets myocardial demand. Hence, with increasing stenosis severity the resistance vessels progressively dilate, leading to a reduction in reserve vasodilator capacity, and therefore to a reduction in CFR. This concept of CFR has been applied to both invasive and noninvasive methods that allow to measure coronary flow or myocardial perfusion, which have consistently shown important prognostic value for this index.32–40 A theoretical issue with CFR, however, is the fact that it is sensitive towards physiological alterations in coronary flow, either during resting or hyperaemic conditions, that are not related to stenosis severity.41 Moreover, it is important to note that CFR incorporates impairment in vasodilator capacity originating from both the epicardial coronary stenosis, as well as potential microcirculatory dysfunction. Therefore, not all reductions in CFR can be attributed to the presence and severity of the epicardial stenosis, and not all impairment of CFR may, therefore, be relieved by PCI. Nonetheless, regardless of the methodology applied, a strong association between CFR and clinical outcomes has repeatedly been observed.22,32,33,35–40 Moreover, CFR has been evaluated against noninvasive standards for myocardial ischaemia, which documented an overall diagnostic accuracy for CFR values ≤2.0 of 81 % to identify stenosis associated with evidence of myocardial ischaemia on noninvasive stress testing.34 Randomised clinical trial data for the use of CFR to guide coronary intervention are, however, not available. All large studies on CFR have either investigated its use to guide the optimisation of coronary angioplasty,42,43 or as part of (large) clinical registries. Together with its relative technical difficulty, especially for ad-hoc evaluation in the catheterisation laboratory, this means that CFR is not widely used as a clinical decision-making tool at this moment. Nonetheless, as will be discussed below, renewed interest into the complex multilevel involvement of the coronary circulation in the setting of IHD has reinvigorated an interest in CFR, leading to the design of large clinical trials to reintroduce CFR in clinical practice.
Coronary Pressure for Stenosis Evaluation
The Basis of Fractional Flow Reserve
Young et al. first introduced the theoretical concept of estimating the impairment of coronary flow due to a coronary stenosis by relating the flow in the coronary artery with the stenosis to that in the same coronary artery without the stenosis.18 This method, however, includes the measurement of coronary flow before and after alleviation of the stenosis and, therefore, unfeasible as a tool to identify haemodynamic stenosis severity before revascularisation. This concept was later expanded upon by Pijls et al., introducing the FFR.5 FFR applies the measurement of proximal and distal coronary pressure during maximal coronary vasodilation to estimate flow impairment due to the stenosis. The FFR framework is therefore based on the assumption that during maximal vasodilation, a proportional linear relationship occurs between coronary perfusion pressure and coronary flow, and that this relationship is the same in the presence and in the absence of a stenosis.11,13 By this assumption, the proximal coronary pressure, or aortic pressure, can be used as an estimate of coronary flow in the absence of a stenosis, and distal coronary perfusion pressure, measured by a pressure-sensing guide wire, can be used to estimate coronary flow in the presence of the stenosis. By expressing the ratio of distal to proximal coronary pressures, FFR reflects the estimated fraction of coronary flow in the presence of the stenosis relative to the situation when the stenosis would be fully relieved (Figure 2).
Clinical Validation of Fractional Flow Reserve
FFR has been evaluated against a multitude of noninvasive tests for myocardial perfusion deficits, which has yielded an overall accuracy of FFR to identify such perfusion impairment of around 81 %.34,44 Moreover, ample randomised clinical outcome data supports the benefit of FFR-guided coronary intervention over the use of the coronary angiogram alone. FFR-guided intervention is associated with equivalent functional and clinical outcomes compared with angiographic guidance, while requiring significantly less revascularisation procedures.6 These findings have led FFR to be incorporated as a dominant diagnostic test in the management of IHD,1 and even has (inappropriately) led several investigators to use FFR as a gold standard reference test for the evaluation of novel tools for IHD management, including advanced noninvasive tests.45 The recent FAME II study results have, however, shed new light on the diagnostic and prognostic characteristics of FFR. This study evaluated routine PCI of FFR-positive stenosis on top of guideline-directed medical therapy versus an approach using guideline-directed medical therapy alone.7,8 Among stenoses with an average FFR of 0.68 ± 0.15, 80 % of medically managed FFR-positive stenosis did not suffer major adverse cardiac events up to two years of follow up, and over 60 % of patients did not require PCI at all during this period. This means that the majority of stenoses that should actually undergo revascularisation according to contemporary clinical guidelines, do not require revascularisation to prevent adverse cardiac events.46,47 Hence, although there is a distinct benefit of FFR-guided revascularisation over PCI-guided by the coronary angiogram, it is not a perfect tool and substantial room for improvement seems to exist.
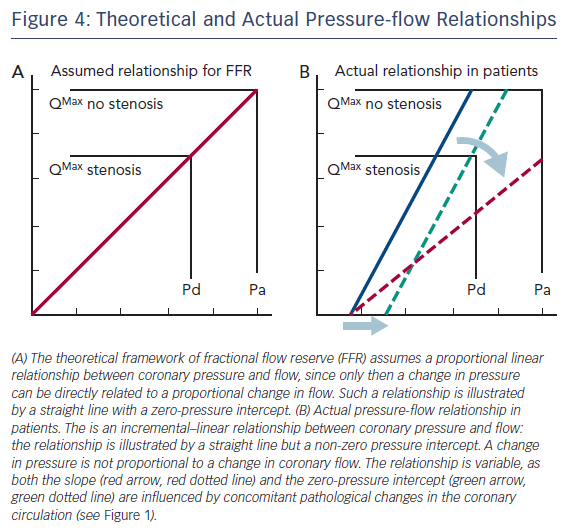
Theory Versus Reality: Accuracy of Fractional Flow Reserve to Identify Flow Impairment
Comparing the theoretical pressure-flow relationship that forms the basis of FFR with the actual pressure-flow relationship in humans illustrates why FFR only provides an estimate of – and is not the same as – stenosis-induced flow impairment in the individual patient (Figure 4).5,10,48,49 First and foremost, in reality the relationship between perfusion pressure and coronary flow is not proportional linear (Figure 4A), but is incremental linear and varies in slope with variation in clinical and haemodynamic conditions (Figure 4B).10,13,49 The variability of the pressure-flow relationship both between patients, as well as within patients between adjacent perfusion territories, means that the deviation of the proportional linear pressure-flow relationship assumed by FFR from the actual relationship in the individual patient is variable as well. Moreover, the FFR-theory assumes that such relationship is the same for unobstructed and stenosed coronaries, which can only occur when coronaries would be rigid pipes that do not change in diameter with a change in perfusion pressure: after all, resistance in the coronary arteries can only be the same in these situations when coronary diameter is independent of perfusion pressure.50,51 However, it is well-known that coronary arteries are pressure-distensible, which precludes the aforementioned assumption and induces another uncertainty regarding the accuracy of FFR to identify actual stenosis-induced flow impairment.52 With such detailed analysis of the assumed and actual pressure-flow relationship, it becomes clear that many factors influence the accuracy with which FFR estimates stenosis-induced flow impairment in the individual patient: it may be very close in some patients, but can be ill-estimated in others. Finally, beyond the conceptual issues with FFR as an estimate of coronary flow impairment, it is important to recall that FFR becomes more abnormal as flow through the coronary artery becomes more normal: an abnormal FFR may therefore coincide with highly normal coronary flow, and vice versa.19,20 Since the myocardium thrives on coronary flow, not on coronary perfusion pressure,21 and coronary flow is the critical determinant of myocardial ischaemia,23,24 such can be interpreted as inaccuracy of FFR to estimate stenotic flow impairment. Clearly, coronary pressure can theoretically be used to estimate coronary flow impairment induced by a stenosis, but it should be realised that many factors interfere with its reliability. Reconciling that the aim of FFR is to identify stenosis-induced flow impairment, which it may misestimate on the basis of basic physiological principles, it becomes clear the limited prognostic value of positive FFR in FAME II may well be explained by misestimated stenosis-induced flow impairment.
The Basis of Instantaneous Wave-free Ratio
The instantaneous wave-free ratio (iFR) is a pressure-derived index of stenosis severity that can be calculated during resting conditions and therefore does not require the use of potent vasodilators in the catheterisation laboratory. iFR is defined as the ratio of distal to proximal coronary pressure during a restricted part of cardiac diastole, termed the wave-free period. This approach means the stenosis pressure gradient is assessed during that portion of the cardiac cycle where coronary flow is intrinsically highest. Thereby, iFR aims to maximise the information on stenosis severity that can be derived during resting conditions. The fact that iFR can be assessed in resting conditions overcomes several ambiguities associated with the use of coronary vasodilators in clinical practice, and simplifies physiological assessment of coronary stenosis severity.
Diagnostic Value of Instantaneous Wave-free Ratio Compared with Fractional Flow Reserve
The diagnostic value of iFR has been evaluated against FFR as the reference standard, as well as against independent reference standards. Overall, iFR agrees with FFR in approximately 80 % of cases.53 When independent reference tests were used to compare the diagnostic efficiency of iFR and FFR, such as CFR assessed with intracoronary Doppler velocity measurements and with PET or invasively assessed hyperaemic stenosis resistance index, no benefit of FFR over iFR could be identified.54–56 Actually, iFR showed better agreement with direct assessment of coronary flow than FFR.57 Hence, both techniques can be considered equivalent alternatives in terms of their diagnostic efficiency to detect haemodynamically relevant coronary stenosis. To date, two large-scale randomised clinical outcome trials comparing iFR-guided versus FFR-guided coronary intervention have been performed: the Functional Lesion Assessment of Intermediate Stenosis to Guide Revascularization (DEFINE-FLAIR) and the Instantaneous Wave-Free Ratio Versus Fractional Flow Reserve in Patients With Stable Angina Pectoris or Acute Coronary Syndrome (iFR-SWEDEHEART) studies. Combining approximately 4,500 patients, these studies documented no difference in the occurrence of major adverse cardiac events between an iFR-guided or FFR-guided revascularisation strategy. Hence iFR and FFR can be considered alternatives for stenosis assessment with respect to clinical outcomes as well. In both the DEFINE-FLAIR and iFR-SWEDEHEART studies, significantly fewer coronary stenoses were identified as haemodynamically significant in the iFR-guided arm compared with the FFR-guided arm, and significantly fewer coronary interventions were performed in the iFR-guided arms.58 Yet, patients deferred from coronary intervention on the basis of iFR had equivalent clinical outcomes compared with patients deferred on the basis of FFR. Moreover, patients with an acute coronary syndrome (ACS) had significantly worse outcomes than the stable coronary artery disease patients (SCAD) in the FFR-guided arm, but not in the iFR-guided arm where outcomes between ACS and SCAD were similar.59 Aside from its proven non-inferiority, iFR induces less patient discomfort since it obviates the use of vasodilators, can be assessed quickly compared with FFR and has the ability to assess serial lesions by performing an iFR-pullback. The latter may be the largest benefit of iFR-guided intervention. In hyperaemic conditions, serial coronary stenoses show interplay as soon as they reach >50 % diameter stenosis: in sequential stenosis, the proximal stenosis will lower blood flow across the distal stenosis and vice versa. When treating either of the stenosis with PCI, coronary flow across the second stenosis will increase, increasing the residual pressure gradient across the residual stenosis. Due to this phenomenon, hyperaemic pressure-wire assessment with FFR does not allow identification of the individual impact of coronary stenosis on the overall FFR-value. In resting conditions, such stenosis interplay does not occur until stenosis severity exceeds >85 % diameter stenosis. Therefore, since PCI does not influence resting flow across the residual stenosis, pre-intervention pressure gradients can be assessed for each individual stenosis. An iFR-pullback, therefore, allows to identify the individual contribution of each stenosis to the overall iFR value, and to optimise planning of the PCI procedure in serial stenoses. Moreover, this iFR scout calculates stenosis severity according to the pressure gradient obtained during the iFR-pullback and predicts real-time potential haemodynamic gain in iFR post-PCI according to stent size.60–62
Improving Identification of True Stenosis Haemodynamic Significance: Combining Fractional Flow Reserve and Coronary Flow Reserve
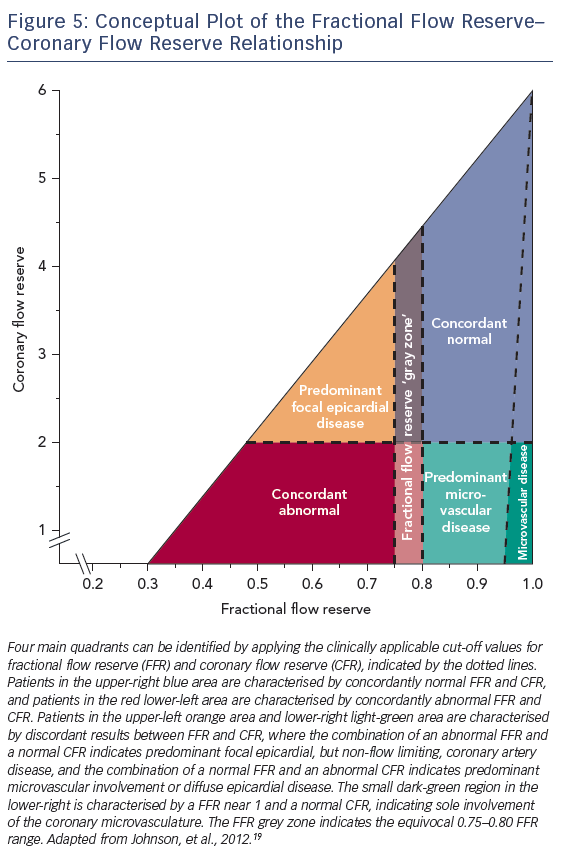
FFR and CFR were long considered alternatives for the physiological assessment of coronary artery disease, and discrepancies between the two have historically been linked to the technical difficulty of obtaining accurate CFR values and the limitations of CFR defined above. Conversely, it has now become evident that FFR and CFR comprise complementary tools, and that discrepancies between the two are the result of basic coronary (patho)physiology.19,20,22,63 Accordingly, the combined interpretation of FFR and CFR allows more accurate discrimination of the pathophysiological substrate in the setting of IHD. The relationship between FFR and CFR is illustrated in Figure 5. On the basis of their clinical cut-off values, four main quadrants can be defined in this relationship. When FFR and CFR are in agreement they are easily interpreted in combination: either no haemodynamically relevant coronary artery disease is present – illustrated by the combination of normal FFR and normal CFR – or there is coronary artery disease that severely impairs coronary flow – illustrated by the combination of abnormal FFR and abnormal CFR. Disagreement between FFR and CFR may arise from distinct (patho)physiological mechanisms. In the presence of a coronary stenosis, the combination of abnormal FFR and normal CFR illustrates the presence of non-flow limiting coronary artery disease. In this situation, the (highly) normal coronary flow through the coronary artery induces a significant pressure drop across the stenosis, leading to an abnormal FFR value. Since the myocardium thrives on coronary flow, not on perfusion pressure, and coronary flow is the critical determinant of myocardial ischaemia, it is the high coronary flow that determines the benign clinical follow up in these patients.20,64 The combination of normal FFR with abnormal CFR illustrates the presence of focal epicardial coronary artery disease superimposed on a background of either microvascular disease and/or diffuse epicardial coronary artery disease. This pattern has been associated with impaired long-term clinical outcomes.20,22 Although it is generally assumed that the normal FFR in this setting reflects that PCI is not applicable in this setting to improve coronary flow, impaired microvascular function may mask haemodynamically relevant coronary stenosis.65 On the basis of this phenomenon, recent case-based clinical data suggests that in select cases, PCI might be a last resort option in an attempt to alleviate the epicardial contribution to coronary flow impairment.66
The combined interpretation of FFR and CFR to optimise decision making is until now only supported by retrospective clinical data. The ongoing Combined Pressure and Flow Measurements to Guide Treatment of Coronary Stenoses (DEFINE-FLOW) study (NCT02328820) aims to evaluate this diagnostic approach in a multicentre prospective observational setting. This study tests the hypothesis that deferral of PCI in stenosis with abnormal FFR and normal CFR leads to equivalent clinical outcome compared with deferral of PCI in stenosis where both FFR and CFR are normal. Such prospective clinical data are needed to ultimately define the role of this approach in clinical practice. This study will similarly provide insight into the clinical relevance of FFR–CFR discordance and its relationship with clinical outcomes.
Combining Pressure and Flow Signals: Calculation of Coronary Resistances
Beyond the combined interpretation of FFR and CFR, the combined assessment of coronary pressure and flow allows for calculation of indices that relate to resistance to coronary flow in the coronary circulation. The resistance in a vascular compartment is defined as the pressure drop across the compartment divided by the flow that goes through it. Accordingly, the maximal resistance to coronary flow induced by an epicardial stenosis can be calculated as the pressure drop across the stenosis divided by distal coronary flow (velocity) during coronary vasodilation. This hyperaemic stenosis resistance index (HSR) was noted to provide significantly higher accuracy to identify stenosis associated with perfusion deficits on nuclear stress imaging than FFR.67 Moreover, it was shown to provide high prognostic value, particularly in those cases where FFR and CFR disagree.68
Together with its strong physiological fundament, these findings have led several investigators to use HSR as a diagnostic reference standard in studies evaluating novel tools for stenosis assessment.69,70 Notably, when calculated during resting conditions, the basal stenosis resistance index also provided very high diagnostic accuracy of at least equivalent magnitude to that of FFR, especially when contemporary guide wires were used that allow measurement of coronary pressure and flow velocity simultaneously.69,71
Clinical Implications and Future Outlook
Above all, the use of FFR has importantly improved the selection of patients that benefit from coronary revascularisation over the use of the coronary angiogram alone. Yet, the robust clinical data documents that further improvement in patient selection should be possible. The complex multilevel involvement of the coronary circulation in IHD means that multimodality physiological evaluation will be required to achieve this goal. As with FFR, it can be assumed that more advanced physiological testing will lead to stricter selection of patients eligible for PCI, reducing unnecessary patient exposure to mechanical revascularisation and improving the benefit of PCI in the individual patient. Yet, this requires the routine measurement of coronary flow in clinical practice, which remains technically challenging. Improvements in the available armamentarium of wire technology are required to make coronary flow measurements feasible, and thereby to provide the opportunity for more complex physiology uptake in clinical practice. Moreover, prospectively gathered (randomised) clinical trial data are needed to further substantiate the relevance of these endeavours for patient outcomes in stable ischaemic heart disease.
Conclusion
In the evaluation of coronary stenosis, coronary pressure and flow both have advantages and disadvantages. Ultimately, both parameters are complementary, and together optimally define the pathophysiological basis of IHD. Although coronary pressure represents the cornerstone of contemporary clinical coronary physiology, evidence is emerging on the clinical relevance of the complex multilevel involvement of the coronary circulation in IHD. More complex physiological testing may well enhance our ability to direct the risk and benefit of mechanical revascularisation to those patients and stenosis that are most likely to benefit. For this purpose, both technical advancement in wire technology and prospective clinical data are needed.