The ancient rite of smoking dates back thousands of years, and tobacco smoking has been largely ingrained in our civilization since the arrival of Europeans to the Americas in the 16th century. For a long time, cigarette smoking was perceived as a symbol of wealth, glamour and sophistication, whereas nowadays it is largely recognised as the first preventable or modifiable cause of common diseases in developed societies.1,2
The prevalence of smoking worldwide is substantial and is associated with a high attributable disease burden. In particular, up to 11.5% of global deaths can be linked to smoking.3 Being decisively fought by every medical association and government organisation, smoking addiction has dramatically evolved in recent times, thanks to the widespread distribution of electronic cigarettes. Consequently, classic cigarette smoking among US adults has declined from 20.9% in 2005 to 15.5% in 2016, as shown in the National Health Interview Survey, while the proportion of those who quit smoking increased by almost 10% from 2005 to 2016.4 However, while a significant decline in cigarette smoking has been reported in the majority of developed societies, the upsurge in electronic cigarettes use is a worrying trend, particularly due to the lack of longitudinal data on their safety and health effects.4
Initially seen as a fancy object, electronic cigarettes have rapidly gained attention both as a tool aiding in tobacco smoking cessation and as a substitute for traditional tobacco addiction. Electronic nicotine delivery systems can emulate the gestures, sensations and pharmacological effects of cigarettes without a strictly defined combustion process. They do so by heating a solution of glycols or glycerol, flavourings and nicotine.
The first electronic cigarette device was patented in the 1930s. The first functioning prototypes were created in the 1960s, but their commercialisation failed. In the early 1980s, Phil Ray, a computer pioneer, along with his physician, Norman Jacobson, revisited and designed a more realistic functioning device, but this had a limited commercial impact. These first devices, merely relying on nicotine evaporation, were perceived as ineffective by conventional tobacco users. After a series of other, mostly unsuccessful, attempts at the dawn of the new millennium, the current version of the electronic cigarette was created in Beijing, China, in the early 2000s, by a smoker pharmacist who rediscovered the device after his father died of smoke-related lung cancer. After being patented in 2004, electronic cigarettes had a strong and steady increase in popularity worldwide.5 They launched in Europe in 2006, and then in the US.5,6 Subsequently, intense and controversial intellectual and legal battles began among supporters and opponents of this emerging smoking lifestyle.
Currently, there is no clear and unequivocal consensus about the health effects of ‘vaping’, as the act of smoking an electronic cigarette is commonly called. Is this a benign trend without detrimental health risks and consequences or is it a wolf in sheep’s clothing?6 The principal goals of this article are to shed some light on the current state of medical and epidemiological knowledge on electronic cigarettes, and to provide succinct and up-to-date information regarding their potential association with cardiovascular risks.
Epidemiology of Electronic Cigarette Usage
In the US, there has been a constant rise in the number of electronic cigarette smokers. The latest data obtained from the National Health Interview Survey showed that 15.3% of adults had repeatedly used an electronic cigarette, while the incidence of active users (defined as at least one electronic cigarette smoked in the past 30 days) was 3.2%. Interestingly, the population that had the highest propensity for the new trend were current tobacco smokers, while former smokers constituted only a small fraction of new vapers; of note, the proportion of non-smokers who started using electronic smoking devices was rather low.7
Recent data from the Behavioural Risk Factor Surveillance System (BRFSS) suggest that the use of electronic cigarettes is increasing among never-smokers, to nearly 2 million US adults in 2016.8 The mean prevalence of never-smokers who smoked electronic cigarettes at least once ranges from 0.1 to 3.8%.7,9,10 Those electronic cigarette users who have never smoked conventional cigarettes are defined as ‘sole electronic cigarettearette’ users in the literature. Of note, electronic cigarettes are unlikely to be a trigger for smoking initiation or relapse among adults in the US.11 A low prevalence of cessation among infrequent electronic cigarette users has been well-documented in a study of recent smokers in the US.12 Similarly, individuals with a positive history of cardiovascular disease who recently quit smoking or reported a recent quit attempt were more likely to use electronic cigarettes compared with current smokers and those who did not report a quit attempt.13
In the EU, 20% of current smokers, 4.7% of former smokers and only 1.2% of never-smokers reported having used an electronic cigarette. Epidemiological data also suggest that electronic cigarette users appear to be younger, more educated, with higher income, and a slight and variable prevalence of men and white people.14 Data from the BRFSS also showed that electronic cigarette use is a common habit, especially among younger adults, current cigarette smokers and people with comorbid conditions.9,10
There is an alarming uptrend in the use of electronic cigarettes among US high school students, with a prevalence ranging from 10 to 13% in 2016.15 In the most recent annual National Youth Tobacco Survey, the Centers for Disease Control and Prevention found that the number of high school students using tobacco, including electronic cigarettes, increased by 38%, with most of the new smokers using electronic cigarettes. In this population, electronic cigarette use increased by almost 78%, with the total prevalence of active vapers reaching 21%, up from 12% in 2017. Importantly, 15% of this population combined vaping and smoking of traditional tobacco cigarettes. According to this report, the use of standard cigarettes and cigars did not increase during the observed period.16 Furthermore, the introduction of JUUL, an innovative electronic cigarette that looks like a USB drive, has seen a rapid uptake among youth and young adults.17 This design provides delivery of high nicotine concentrations, while the potential health hazards associated with this product are unknown.18 The most recent report by Bold et al. revealed that electronic cigarette use among young people in public schools was associated with future cigarette use during the three-wave period (2013, 2014 and 2015), whereas cigarette use was not associated with future electronic cigarette use.19 In contrast, according to large-scale surveys and cross-sectional analyses of randomised controlled trials, the majority of electronic cigarette users perceive these devices as a tool to quit regular tobacco smoking.20,21
How do Electronic Cigarettes Work?
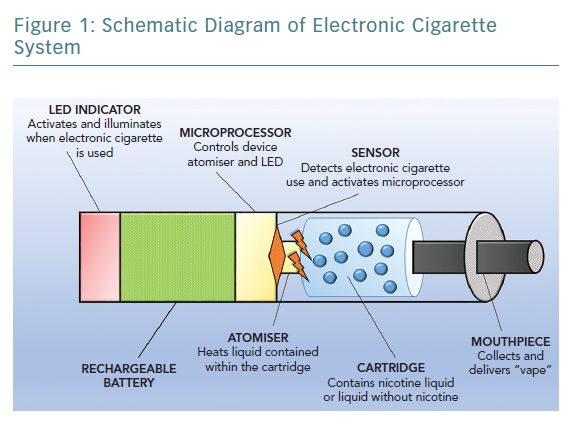
These devices try to mimic the experience of smoking by resembling the shape of a conventional cigarette. The most common type of electronic cigarette cartridge contains a propylene glycol or glycerol solution, with or without added nicotine, and generally with a flavour. Heating the compound creates a resistance within the cartridge, generating a vapour that is inhaled by the user. The basic functioning unit of electronic cigarettes is shown in Figure 1. Thousands of flavours are available, and health concerns exist about the potential role and effects of these chemicals. Almost more than 8,000 unique flavours and more than 450 brands of electronic cigarettes have been reported, with limited data suggesting that these substances are potentially detrimental to human health; many of these substances are known irritants or can increase susceptibility to viral infections.22–24 As a consequence of the structure of the device itself, many different heavy metals, such as chromium, manganese and even arsenic, have been reported to be detected in electronic cigarette liquids and aerosols. Moreover, combustion is not part of the process, combustion-related compounds have been detected in electronic cigarette smoke, including nitrosamines, organic acids and phenolic compounds.25,26
The average nicotine concentration per cartridge is usually <36 mg/ml, with the most common variants ranging from 6 to 18 mg/ml. Importantly, some biochemical analyses have shown that most of the devices actually provide an effective dose of nicotine that is higher than the concentration declared on the label, while some nicotine-free cartridges were found to deliver nicotine.27,28 Furthermore, it has been documented that more experienced users, who exhibit longer and more frequent aspirations, have higher blood nicotine levels compared to classic tobacco smokers, whereas less experienced users have consistently lower levels of nicotine in their circulation.29–31 Therefore it can be seen that these novel electronic cigarette systems allow users to regulate the amount of nicotine they inhale, thereby raising a valid concern regarding nicotine abuse and its addiction potential.32 Furthermore, vaping low-nicotine versus high-nicotine e-liquid in electronic cigarettes is accompanied by an increase in wattage and larger quantities of potentially harmful e-liquid consumption.33
As the use of alternative nicotine delivery products is increasing worldwide and may surpass the use of conventional cigarettes in some parts of the world, it is a pertinent research question to elucidate the explicit role of nicotine in the development of cardiovascular and other systemic diseases. Recently, nicotine has been implicated in the impairment of vascular function, endothelial dysfunction and increased vascular calcification and stiffness.34
Potential Health Harms of Electronic Cigarettes Unrelated to Cardiovascular Risk
No long-term observational data exist about the health effects of these technologies on human health. However, it is an intuitive concept that electronic cigarettes should present fewer health risks than traditional cigarettes.35 In support of this notion, a recent study by Goniewicz et al. demonstrated that substituting tobacco cigarettes with electronic cigarettes may result in significantly lower exposure to the wide array of toxins and carcinogens that are present in tobacco, thus suggesting a role of electronic cigarettes as a potential harm reduction device.36 One study has shown that electronic cigarette smokers have fewer toxins and carcinogens in their urine compared with conventional cigarette smokers.37,38 Nonetheless, the health-related effects of the vapour fumes are unknown, and the levels of carcinogenic compounds found may vary, largely due to the heterogeneity of the available commercial products.
It is known that at high temperatures, propylene glycol may form propylene oxide, a probable human carcinogen, while glycerol produces acrolein, which is a known human toxin.39 Importantly, both of these substances constitute the major ingredients of most refill solutions, and can form formaldehyde and acetaldehyde, which are both established human carcinogens.40–43 Electronic cigarettes also produce aerosols that include polycyclic aromatic hydrocarbons, nitrosamines and silicate particles, which are well-documented carcinogens.44–47 Detrimental carbonyl content was significantly increased in exhaled breath during electronic cigarette use compared with non-vaping users.46 The effects of artificial flavours are similarly uncertain. Some studies suggest a link between some chemical compounds used to emulate specific sweet tastes and respiratory irritation and cytotoxicity.23,48
Current data generally suggest a varying detrimental effect of electronic cigarettes on the inner mucosa of the craniofacial region and respiratory function when compared with standard tobacco, with an especially strong association with asthma.49–51 This association was documented in two independent surveys carried out among teenage electronic cigarette users with a risk of bronchitis symptoms directly related to the frequency of electronic cigarette usage.46,52,53
Detrimental acute effects of electronic cigarettes inhalation were demonstrated in a study conducted by Antoniewicz et al. among 17 healthy individuals, which showed that inhaled electronic cigarette aerosol with nicotine caused a significant increase in heart rate and arterial stiffness, and a sharp increase in flow resistance in the conducting airways.54 Similarly, acute vaping of propylene glycol/glycerol aerosol at high wattage with or without nicotine induced significant injury to airway epithelium and impaired pulmonary gas exchange.55 Electronic cigarettes also induce an ion channel dysfunction in airway epithelial cells, and this was partially explained by the increased acrolein production, thus associating electronic cigarette use with chronic bronchitis onset and progression, as well as chronic obstructive pulmonary disease severity.56
Additionally, electronic cigarettes induced a greater efflux of inflammatory mediators from chronic obstructive pulmonary disease lung cells, implicating that the use of electronic cigarettes in chronic obstructive pulmonary disease might be associated with a worse clinical picture and exacerbations.57 Oral gum disease has also been associated with electronic nicotine products, with electronic cigarette users having an increased odds of being diagnosed with gum disease and bone loss around teeth (OR 1.76, 95% CI [1.12–2.76] and OR 1.67, 95% CI [1.06–2.63], respectively), compared with non-smokers.58 Among university students, vaping was associated with illicit drug use, mental health problems and impulsivity.59 Finally, a preclinical study showed that electronic cigarette vapours impaired gonadal function in male rats, although this early finding is yet to be confirmed in human studies.60
Electronic cigarettearettes as a Road to Quit Cigarette Addiction
The role of this technology in the difficult path to quitting smoking addiction has been postulated and investigated in small-sized studies. By looking and tasting like traditional tobacco and, moreover, by allowing the social rite of smoking as well as the physical hand-to-mouth gesture, electronic cigarettes could indeed be more effective than other smoking cessation strategies.
Preliminary evidence suggests that electronic cigarettes can reduce tobacco cravings and nicotine abstinence symptoms.30,61 A survey study conducted in the US found that electronic cigarette smokers had a higher probability of succeeding in quitting (8.2% versus 4.8%), compared with smokers who did not use electronic cigarettes.62 A small study conducted in Italy demonstrated a cessation rate of 12.5% among electronic cigarette smokers after 24 months.63 This favourable trend is still debated, because other studies have failed to prove a higher rate of quitting. Recently a large meta-analysis found 28% (OR 0.72, 95% CI [0.57–0.91]) lower odds of quitting smoking in patients who used electronic cigarettes compared with those who did not use electronic cigarettes.64–66
In a very recent article by Hajek et al., a pragmatic randomised controlled trial with nearly 1,000 smokers motivated to quit smoking was reported. 67 Participants were randomised to either electronic cigarettes containing nicotine at 18 mg/ml or to a nicotine-replacement product, both accompanied with behavioural support. The results indicated that electronic cigarettes were more effective than standard replacement therapies considering the rate of abstinence at 1 year, although the overall success rate was poor in both examined groups (<1 in 5 for electronic cigarettes and <1 in 10 for nicotine replacement).67 An interesting observation from this trial was that, among participants with sustained abstinence at one year, the cumulative incidence of continued electronic cigarette use was much higher among those that were randomised to electronic cigarettes compared with those that continued to use nicotine replacement in the nicotine-replacement group (80% versus 9%, respectively).68
This important finding further reinforces the need to ascertain potential health consequences of long-term electronic cigarette use. Furthermore, there is also a tangible concern about the role of electronic cigarettes as a bridge towards a classical tobacco addition. A systematic review and meta-analysis of epidemiological studies comprising thousands of US young adults, and a subsequent prospective study, showed that initiation of cigarette smoking is more common among previously electronic cigarette users compared with previous cigarette non-users.69,70 A huge variety of available refill flavours certainly impose a potential to enhance the appeal to novice users, making the initial exposure more pleasurable and perhaps more likely to occur
Electronic Cigarettes and Cardiovascular Risks
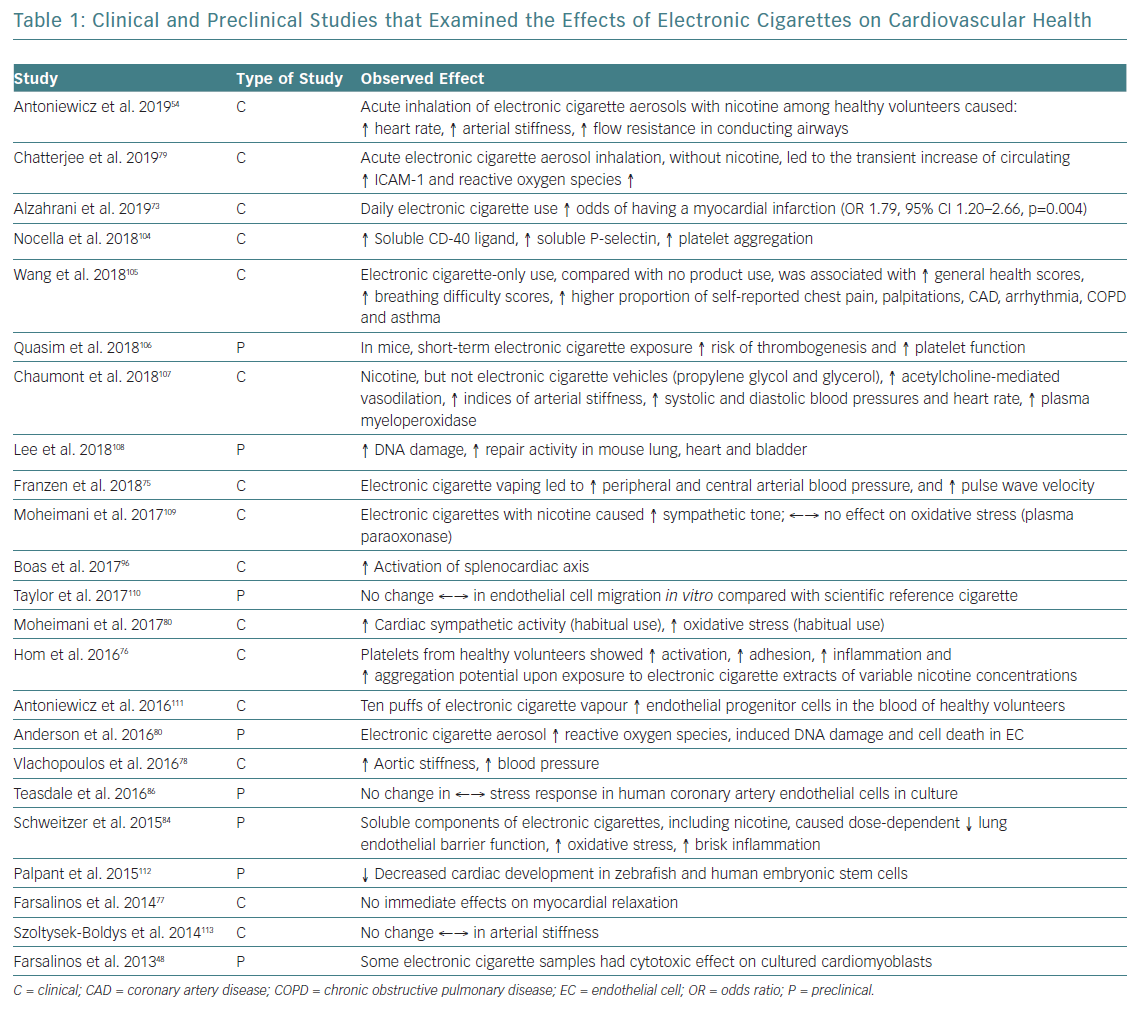
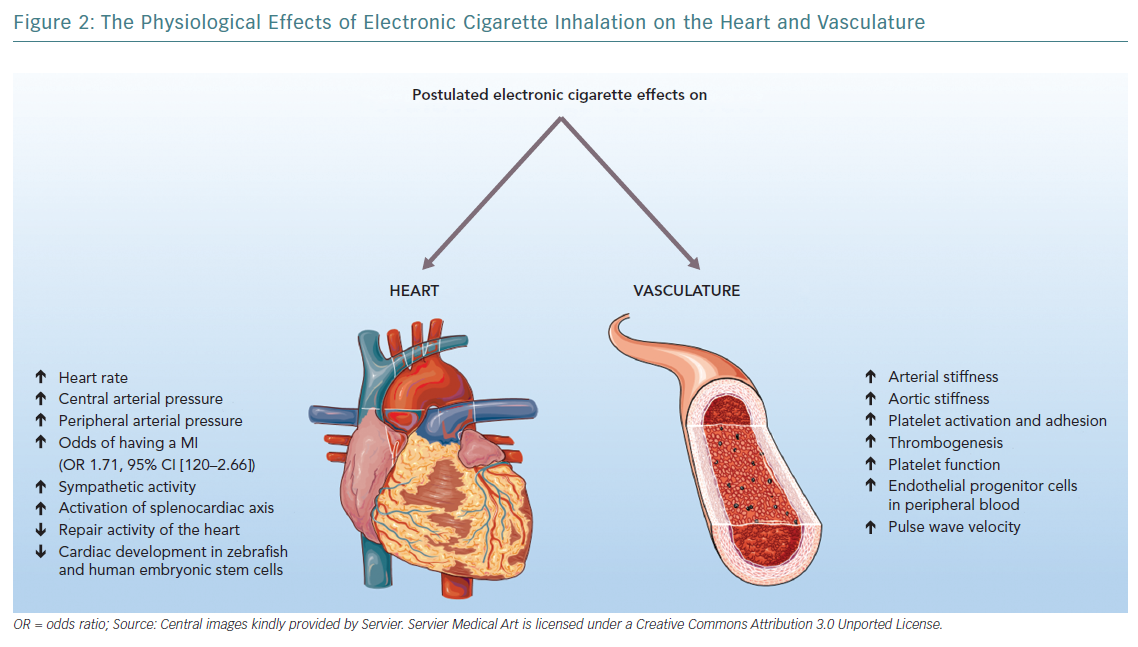
There is no consensus about the effects of electronic cigarettes on the cardiovascular system, with most of the available data coming from preclinical studies. The effects of electronic cigarettes on cardiovascular health are summarised in Table 1, while postulated effects on the heart and vasculature, mainly derived from preclinical studies, are shown in Figure 2.
In a large cross-sectional analysis conducted among a US population, electronic cigarette use was associated with lower general health status, higher breathing difficulty scores and greater incidence of cardiac symptoms, such as chest pain, palpitations, arrhythmias or coronary artery disease.71 Very recently, in a cross-sectional analysis of 400,000 adult respondents from the 2016 BRFSS survey, almost 70,000 people reported electronic cigarette use, and this was associated with a 71% increased risk of stroke, 59% higher risk of acute MI and a 40% higher risk of angina and coronary artery disease; moreover, they had twice the risk of switching to regular cigarettes.72 Similarly, in a recent logistic regression analysis performed among the National Health Interview Surveys 2014–2016 population, daily electronic cigarette use, after adjusting for conventional tobacco exposure and other risk factors, was significantly associated with a 79% increase in the odds of suffering an acute MI.73 In contrast, pooled data from the BRFSS 2016–2017 sample that included almost 450,000 participants failed to find a significant association between sole electronic cigarette use in never-smokers and cardiovascular disease, whereas dual use of electronic cigarettes and combustible cigarettes was associated with a 36% higher odds of cardiovascular disease compared with tobacco smoking alone.74
Limited data currently exist regarding the general cardiac effects of electronic cigarette smoking. After vaping one electronic cigarette, an acute and significant rise in peripheral arterial pressure was observed together with a steep increment in heart rate, and both changes lasted up to 45 minutes.75 It has also been demonstrated that, among healthy electronic cigarette users, heart rate variability shifted towards a sympathetic predominance with the decreased vagal tone, which are both risk factors of cardiovascular mortality. Interestingly, these effects were unrelated to nicotine, as its plasma levels were virtually undetectable.76
A study used transthoracic echocardiography to evaluate LVF before and after smoking one tobacco cigarette or vaping an electronic cigarette for 7 minutes with a refill that had a medium-strength nicotine concentration. It was found that while baseline parameters were comparable in both groups, after regular tobacco cigarette use, participants had higher Myocardial Performance Index, prolonged isovolumic relaxation time, and decreased diastolic strain rate and mitral annular early diastolic velocity, thus indicating a relevant diastolic impairment. In contrast, electronic cigarette users had no significant changes in immediate haemodynamic parameters of both systolic and diastolic function.77
In a small prospective study, electronic cigarette smoking for >30 minutes (which is considered comparable to classic cigarette smoking for >5 minutes) induced an unfavourable acute effect on aortic stiffness and blood pressure, which are known predictors of cardiovascular risk and all-cause mortality.78 In terms of acute effects of electronic cigarette aerosol inhalation in healthy subjects, one study revealed a transient increase in oxidative stress and inflammation parameters, thus suggesting that electronic cigarette exposure without nicotine might drive the onset of vascular pathologies through reactive oxygen species and immune cell adhesion pathways.79 Similarly, a small clinical study by Antoniewicz et al. demonstrated that inhaled electronic cigarette aerosols with nicotine had an acute negative impact on vascular and pulmonary function.54
An in vitro study by Farsalinos et al. showed that the extract from electronic cigarettes (containing different flavours and nicotine quantity) applied to cultured myocardial cells at different dilution, both with or without nicotine, was cytotoxic at different concentrations irrespective of nicotine presence. The base solution consisting of glycerol and propylene glycol was not found to be cytotoxic at any concentration.48 These results seem to suggest that the toxic effects of electronic cigarettes could be elicited by the added flavours.
In a similar experimental study, the application of aerosol extracts from electronic cigarettes on vascular endothelial cells for at least 4 hours induced a significant escalation in reactive oxygen species generation, causing DNA damage and reducing cell viability in a dose-dependent manner. Both apoptosis and programmed necrosis pathways were upregulated; moreover, treatment with alpha-tocopherol and n-acetylcysteine, which have recognised anti-oxidant properties, provided a partial rescue of these cells, thus suggesting the involvement of reactive oxygen species in this pathological cascade.80
The potential interference with thrombosis and inflammation mechanisms was suggested by another study showing that exposing platelets to electronic cigarette vapour extracts induced a significant upregulation of the pro-inflammatory complementary elements C1 and C3b, even higher than traditional tobacco smoke extracts, and was accompanied with a concomitant boost in platelet activation, aggregation and adhesion capacity. These effects were independent of nicotine concentration, as the presence of pure nicotine extract resulted in the inhibition of platelet functions, suggesting that maybe other constituents of electronic cigarettes can antagonise normal platelet function; nonetheless, the presence of nicotine could somehow perpetuate platelet functional changes in a dose-dependent manner, making its role in electronic cigarette-induced damage even more inconclusive.81
Another link to cellular dysfunction induced by vaping was provided by a study analysing the response of liver Kupffer cells both to classic and electronic cigarette extracts exposure. In both cases, a strong inflammatory response was elicited, paired with increased oxidative stress and systemic cytokine release, which likely affected platelet function and general circulatory homeostasis.82
Platelet function seems to be modified by electronic cigarette vapours. In a mouse model of electronic cigarette exposure, platelets that were exposed to electronic cigarettes were more hyperactive, with a greater propensity towards aggregation induced by dense alpha granules secretion, and activation of alphaIIb-beta3 receptors and protein kinase B-extracellular signal-regulated kinase pathways.83 Moreover, these cells were also less sensitive to prostacyclin-induced inhibition when compared with clean air-exposed cells. These changes could theoretically increase the overall risk of thromboembolic events.
Other evidence of the possible irritant and inflammatory effect on cells comes from an in vitro study in which the exposure of tracheobronchial cells to electronic cigarette nicotine-free vapours was related to a concomitant increase in interleukin-6 and interleukin-8 cytokine production with a dose-dependent response and direct evidence of endothelial dysfunction.84 The association with inflammation and endothelial dysfunction is most likely mediated via nitric oxide pathways; although to a lesser degree than standard cigarettes, electronic cigarettes lead to an important increase in soluble nicotinamide adenine dinucleotide phosphate oxidase 2-derived peptides and a concomitant decrease in nitric oxide bioavailability.85 Nonetheless, in human coronary endothelial cells, tobacco smoke, but not electronic cigarette aerosols, was shown to induce nuclear factor erythroid 2-related factor 2 oxidative stress sensing factor transcription.86
In another study, exposure of umbilical endothelial vein cells to electronic cigarette compounds induced cytotoxic pathways, inhibited cell proliferation and altered cellular morphology when compared with regular tobacco.87 An animal study suggested that electronic cigarettes could also hamper metabolic homeostasis. Experiments on 14-day-old mice showed that those exposed to electronic cigarettes had lower bodyweight compared with non-exposed mice, irrespective of nicotine concentration. Furthermore, these vapours could elicit persistent behavioural changes later in adulthood.88
A recent study focused on the new device subtype of the heat-not-burn tobacco cigarettes (IQOS in particular), also casting shadows on the potential toxic effect of these products. After 72 hours of exposure to the aerosols generated by heat-not-burn devices, both bronchial epithelial cells and smooth muscle cells suffered a loss of viability, and an increase in lactate dehydrogenase release, collagen I and fibronectin, with a detrimental effect on the mitochondrial respiration chain. Notably, many of these effects were achieved with lower concentrated aerosols than the aerosols produced by standard electronic cigarettes.89
Concerns about cardiac adverse events also directly involve nicotine, which is found at the same concentration in the blood of experienced electronic cigarette users as classic smokers. Nicotine has known pathological effects, mainly related to the excessive release of catecholamines, endothelial dysregulation and increased insulin resistance.90 Nicotine in electronic cigarettes has been shown to increase heart rate after overnight abstinence.91
Regarding lipid metabolism, nicotine in electronic cigarettes has been shown to increase the amount of circulating saturated fatty acids, decreasing the content of unsaturated fatty acids and inducing insulin resistance. Nicotine can also promote endothelial dysfunction, inhibit cellular apoptosis and enhance angiogenesis, thereby raising concerns about its possible role in the pathophysiology of atherosclerosis and even cancer development.92,93 Interestingly, in another experiment, rats exposed to electronic cigarette refill liquid had better metabolic profiles, with decreased total cholesterol, low-density lipoprotein cholesterol and low-density lipoprotein:high-density lipoprotein ratio. However, caution is required in interpreting these results, as this perceivable benefit was accompanied with a significant elevation in liver enzymes, thus establishing these apparently beneficial changes as a mere reflection of the toxic damage of electronic cigarette liquid on the liver.94
Recently, electronic cigarettes have been proposed as a possible interfering factor in the splenocardiac axis, a signalling network involving the brain, autonomic nervous system and hematopoietic tissues. Of note, after suffering acute stress, a sympathetic activity can cause efflux of leukocytes and progenitor cells from the bone marrow and spleen; these cells subsequently enter the arterial wall and promote atherosclerosis.95 In young adults who chronically used electronic cigarettes, FDG-PET CT showed increased uptake in the spleen and aortic wall compared with non-users, which is consistent with the engagement of the splenocardiac axis by the substances released by these devices.96
The effect on physical properties of the cardiovascular system come from a study of mice exposed to electronic cigarette vapours for 8 months (4 hours a day for 5 days a week, emulating an equivalent of 20 years of exposure in humans). This resulted in a 2.5-fold increase in aortic stiffness, a 24% lower maximal aortic relaxation in response to methacholine and a trend towards a reduction in left ventricular ejection fraction.97 Nonetheless, in humans, it seems that electronic cigarettes could be less harmful than standard cigarettes, as hypertensive patients who switched to electronic cigarettes benefited from a reduction in mean arterial blood pressure and improved pressure control.98
It should be emphasised that most of the data on the cardiovascular effects of electronic cigarettes are derived from preclinical, cross-sectional or small-sized clinical studies in which standard cigarettes were used as a comparison arm, thus providing limiting and conflicting results. A large majority of such studies were also not designed to infer causality. Furthermore, most of these studies focused on the acute effects of electronic cigarette exposure, whereas it is unknown how and if these effects would translate to chronic and longitudinal electronic cigarette use. Likewise, population-wide studies have been confounded by combustible cigarette use, thus making the effect of electronic cigarettes alone challenging for interpretation.
Another important issue is the varying pattern of electronic cigarette use among different groups; for example, dual users of electronic cigarettes and combustible cigarettes, former smokers, and never-smokers that use electronic cigarettes. Even within the electronic cigarette smoking population, the large heterogeneity of available electronic cigarette products, different nicotine concentrations and varying levels of daily exposure pose a real difficulty in ascertaining the true effect of electronic cigarettes on general and cardiovascular health.
It should also be noted that the National Academies of Sciences, Engineering, and Medicine in 2018 released a report summarising available evidence regarding the public health consequences of electronic cigarette use.99 That report concluded that there is no available evidence as to whether or not electronic cigarette use is associated with clinical cardiovascular disease outcomes and subclinical atherosclerosis. Due to this, further investigation is warranted, as the long-term and longitudinal impacts of electronic cigarettes on cardiovascular health at the present moment remain unclear.
Regulatory Approval of Electronic Cigarettes
Regulatory approval of electronic cigarettes varies by country and is constantly evolving to preserve public health interests, as data build up. On a global scale, the WHO suggested stopping the promotion of electronic cigarettes to non-smokers and young people, and restricting the possibilities of advertising and indoor use.100 Likewise, the American College of Preventive Medicine’s Prevention Practice Committee recently issued a consensus-based statement recommending that electronic nicotine delivery systems should be screened in the general population, with special emphasis on electronic nicotine delivery systems initiation prevention among youth, but also in smokers intending to quit.101
In 2016, the US Food and Drug Administration (FDA) firmly regulated cigarettes and smokeless tobacco, including electronic cigarettes, prohibiting their sale to teens and even distribution of free samples. However, it allowed commercialisation of flavours and did not impose restrictions on electronic cigarette advertisements. The current FDA regulations also bind manufacturers to submit an application to list the chemicals inside the devices and to prove that their products respect relevant safety standards. Besides FDA indications, many US states have banned the use of electronic cigarettes in areas where traditional smoking is already forbidden.
It is an interesting fact that in the largest coordinated enforcement effort in the FDA’s history, the agency issued more than 1,300 warning letters and fines to retailers that illegally sold JUUL and other electronic cigarettes brands to minors.102 This phenomenon shows that there are substantial challenges involving the legal regulation and on-market monitoring of these products. The European Parliament approved a directive that limits the maximum amount of nicotine in electronic cigarettes; products containing >20 mg/ml of nicotine are regulated as medical devices.
Finally, as traditional smoking is forbidden in public places in most developed societies, resulting in a tangible reduction in smoking prevalence in the US, it has been postulated that electronic cigarettes could ‘renormalise’ the smoking habit, thus jeopardising the social perception of health risks imposed by tobacco products.103
Conclusion
To date, there is no conclusive and clear data on the effects of electronic cigarettes on cardiovascular and general health, especially from a longitudinal perspective. While waiting for more evidence, it seems reasonable to consider electronic cigarettes as a better option when compared with conventional tobacco products, but at the same time it should be fairly obvious that no smoke is better than electronic smoke.